Non-sterile Product Testing
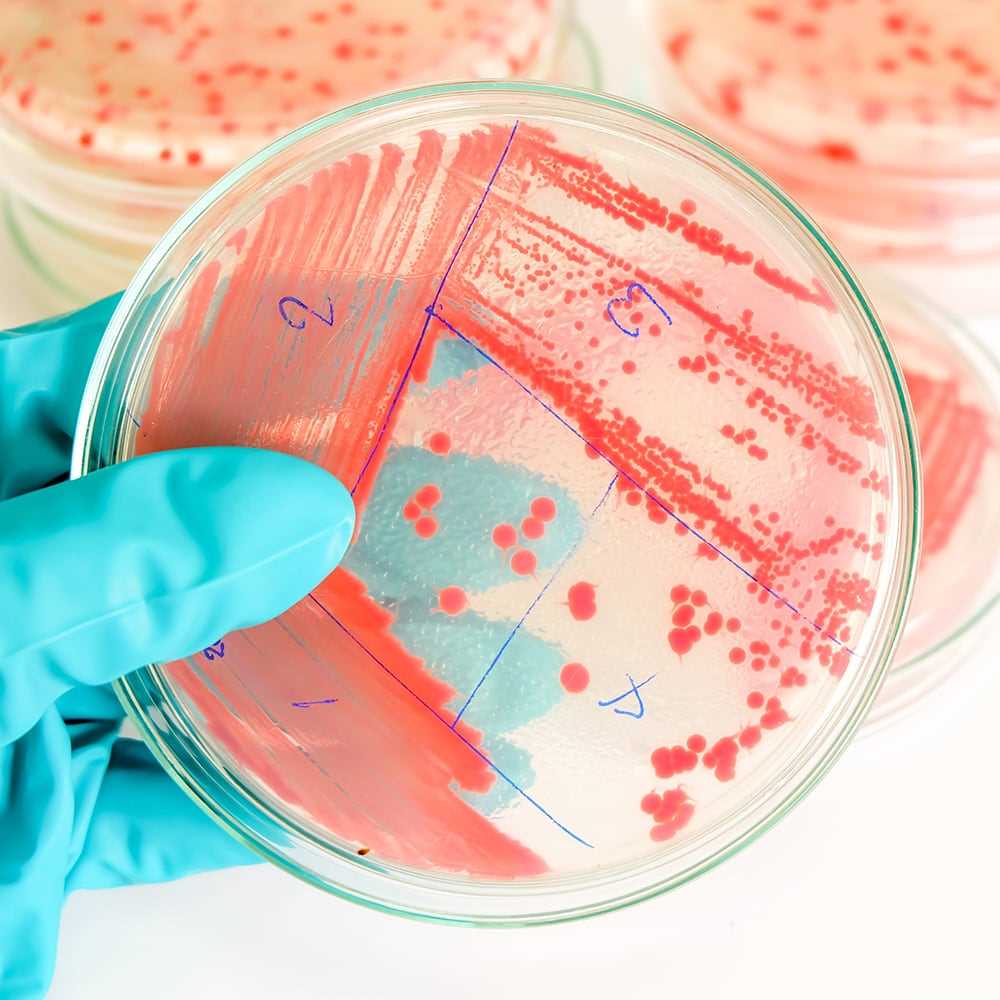
Testing is supported in line with the harmonized compendial requirements for the Microbiological Examination Of Non-sterile Products and the Tests for Specified Microorganisms, typically by the Membrane Filtration or Plate-count methods. ALS performs method suitability assessments of the selected test methods, demonstrating recovery of micro-organisms in the presence of product, ahead of routine testing.
ALS routinely handles a broad range of sample matrices, including harsher antibiotics, API’s, disinfectants and preservative-laden aqueous formulations, which can necessitate neutralisation for the removal of antimicrobial activity paralleled to scientific demonstration of absent neutralizer toxicity. The suitability of the counting method must be demonstrated in the presence of product.
All ALS facilities strive to achieve industry best practice inclusive of recommendations set out in USP Chapter <1117> amongst others. While not exhaustive, Compendia acceptance criteria for the microbiological quality of non-sterile dosage forms is principally defined by the route of administration backed by risk-based impact assessments as referenced in USP <1111>. The need for additional controls of objectionable microorganisms should be determined for each product. Alternative criteria is applicable to drug substances, herbal medicines and dietary supplements although in any case, typical requirements include:
Microbial Enumeration Tests
- Total Aerobic Microbial Count (TAMC)
- Total combined yeasts and molds count (TYMC)
Specified Micro-organisms
- Staphylococcus aureus
- Pseudomonas aeruginosa
- Escherichia coli
- Salmonella
- Candida albicans
- Bile-tolerant Gram-negative bacteria (BTGN)
- Clostridia
- Burkholderia cepacia (BCC)
Whilst compendia are harmonized for most non-sterile dosage forms, testing is conducted in accordance with:
- USP ⟨61⟩ Microbiological Examination of Nonsterile Products: Microbial Enumeration Tests
- USP ⟨62⟩ Microbiological Examination of Nonsterile Products: Tests for Specified Microorganisms
- Ph. Eur. method 2.6.13 Microbiological Examination of Non-sterile Products
- Ph. Eur. method 2.6.12 Microbial Enumeration Tests
ALS can include further specified and objectionable microorganisms into testing regimes, such as isolates from environmental monitoring, where known risks persist.
Other test methods, including rapid microbiological methods, may be used for product testing, but will require validation to demonstrate their suitability and equivalence to the compendial methods. As Technical Projects, ALS can support the development and validation of alternative procedures.
Water Activity Determinations can be supported per USP <922> and Ph. Eur. 2.9.39 methods.
 Search
Search
 English
English
 Login
Login